Resources
The State of Healthcare Patient Communication in 2026

Patient communication is a critical part of the healthcare experience, and it can shape whether someone feels supported, informed, and willing to follow through on care. But that experience doesn’t just happen in the exam room. It shows up in every text reminder, portal message, phone call, and email a patient receives.
Ahead of 2026, Sinch Engage surveyed 1,000 patients across the U.S., ranging in age from 18 to 78 years old, to better understand how text communication impacts behaviors like appointment attendance and prescription refills. The research explores:
- where patients see value in two-way messaging
- when patients expect to interact with a real person vs. AI
- patient’s comfort level for AI-driven communication for healthcare use cases
- the growing role of text messaging in patient expectations
At a broader level, the findings offer a snapshot of how patient–provider communication is evolving and where healthcare organizations have the greatest opportunity to meet patients where they are.
Keep reading as we dive into the survey results and find out how healthcare communication can be improved in the new year.
Key healthcare SMS marketing statistics
- 93% of patients have opted in to receive texts from their healthcare providers and facilities in 2026.
- Texting has now surpassed email and patient portals as patients’ preferred form of communication in healthcare.
- 42% of Gen Z patients would switch providers or pharmacies if they didn’t offer texting.
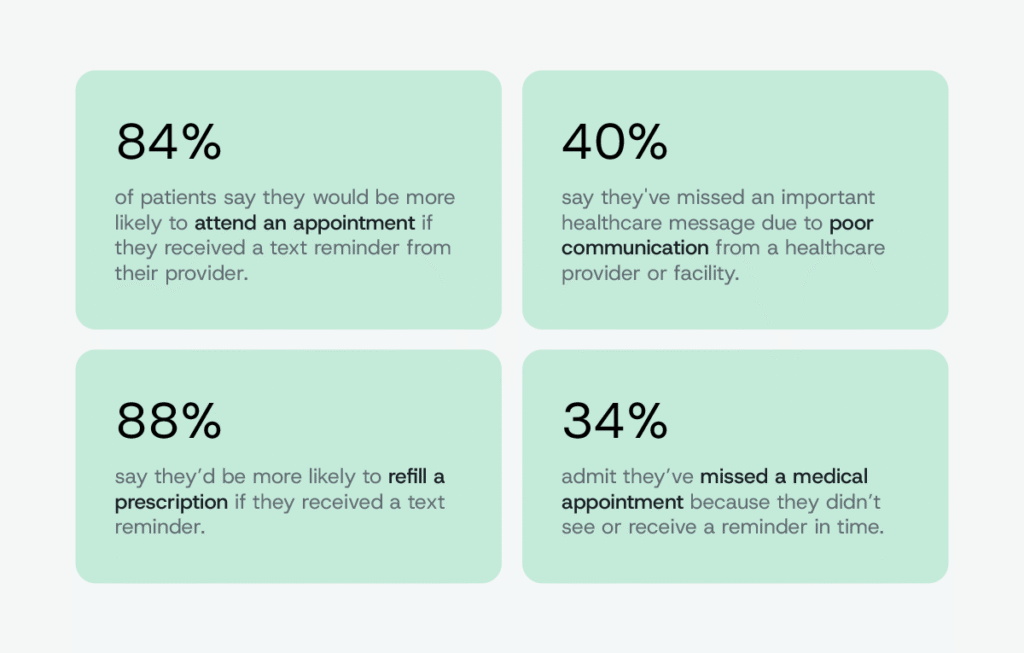
- Healthcare SMS reduces no-shows: 84% of patients say they’re more likely to attend an appointment if they receive a text reminder from their provider.
- Patient text messaging boosts prescription refill rates: 88% say they’re more likely to refill a prescription if they received a text.
- Most patients (68%) want two-way texting where they can ask providers simple questions or confirm/reschedule appointments.
- More than half of patients (55%) are comfortable with AI in patient text messaging as long as it’s used for simple reminders, but they draw the line at personal or sensitive conversations.
- 43% of patients say they saved between one hour and more than three hours over the past year by texting with their healthcare providers and pharmacies instead of calling.
Healthcare SMS opt-in rates are nearly universal
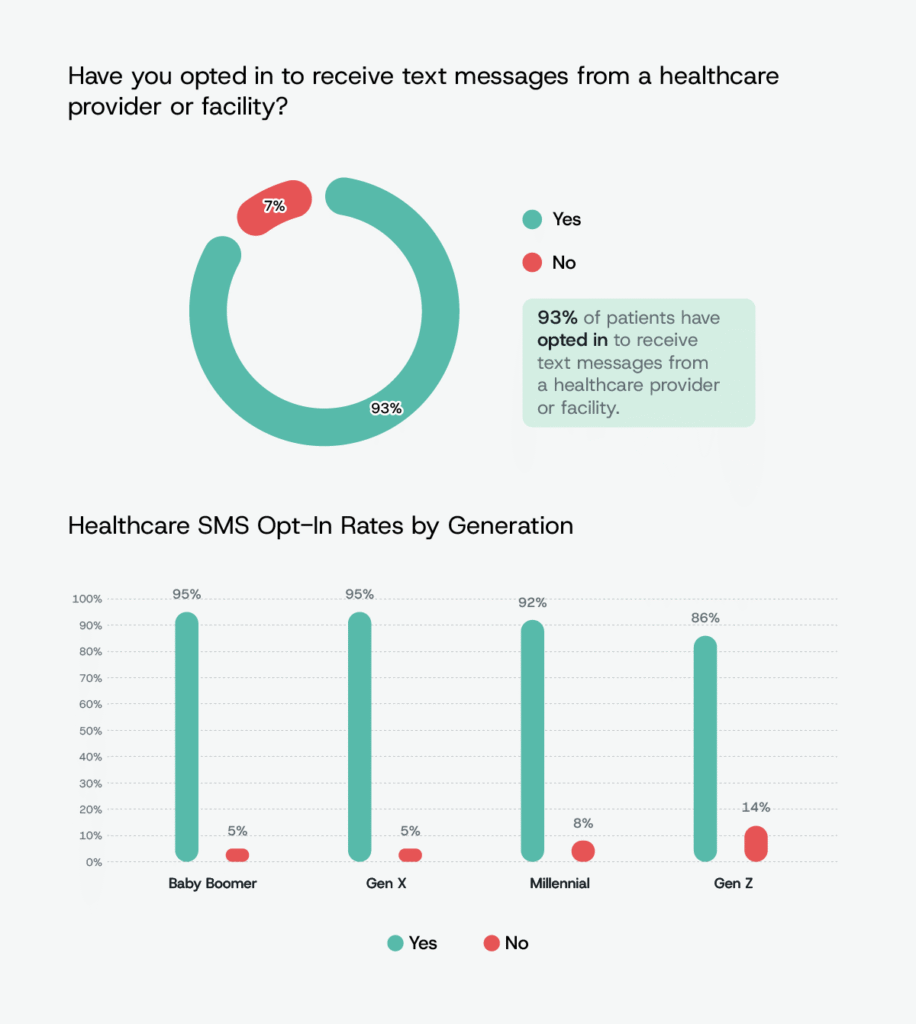
When we asked patients whether they had opted in to receive text messages from a healthcare provider or facility, an overwhelming 93% of Americans said yes. The result highlights how commonplace healthcare SMS has become across the U.S., with opt-in no longer representing a meaningful barrier for most providers looking to communicate with patients by text.
Gen Z stands out as the generation least likely to receive healthcare texts. 86% of them have opted in to healthcare texts, while 14% have not. This gap appears to be driven less by reluctance to receive texts and more by differences in healthcare utilization, as younger adults tend to have fewer appointments with providers and therefore fewer opportunities to enroll in text-based communication in the first place.
Convenience wins: patients choose texting to avoid phone tag and missing emails
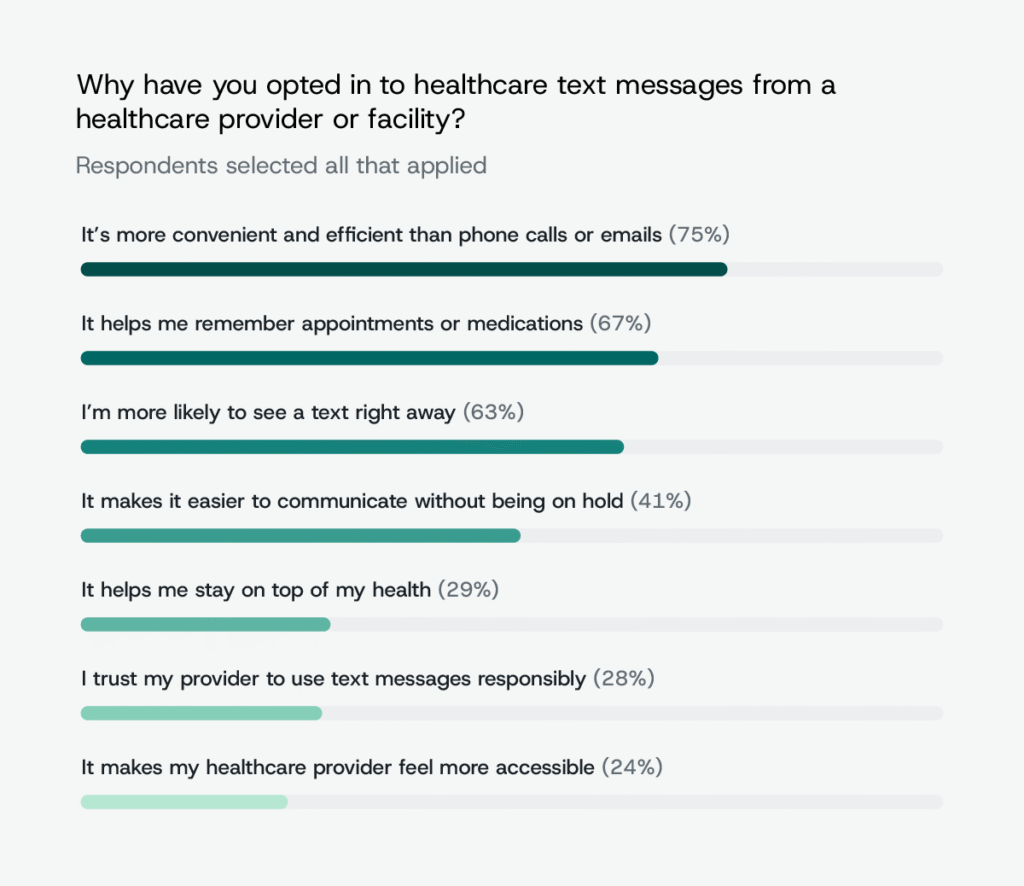
To understand why patients opt in to SMS for healthcare in the first place, we asked respondents what motivates their decision to receive texts from providers and facilities. Convenience emerged as the driving factor, with 75% of patients saying they opted in because texting feels more efficient than phone calls or emails. Rather than viewing SMS as a novel channel, patients largely see it as the easiest way to manage routine healthcare interactions without adding friction to their day.
67% say they opt in because text messages help them remember appointments or medications, reinforcing SMS as a built-in reminder system rather than just a communication tool. Speed plays a similarly important role, as 63% of respondents say they choose texting because they are more likely to see a message quickly, while 41% opt in to avoid long hold times on the phone.
In contrast, fewer patients cite trust (28%) or a sense that their provider is more accessible (24%) as primary reasons, suggesting that efficiency and immediacy outweigh relational factors when it comes to channel preference.
Texting surpasses phone calls and patient portals for patient communication
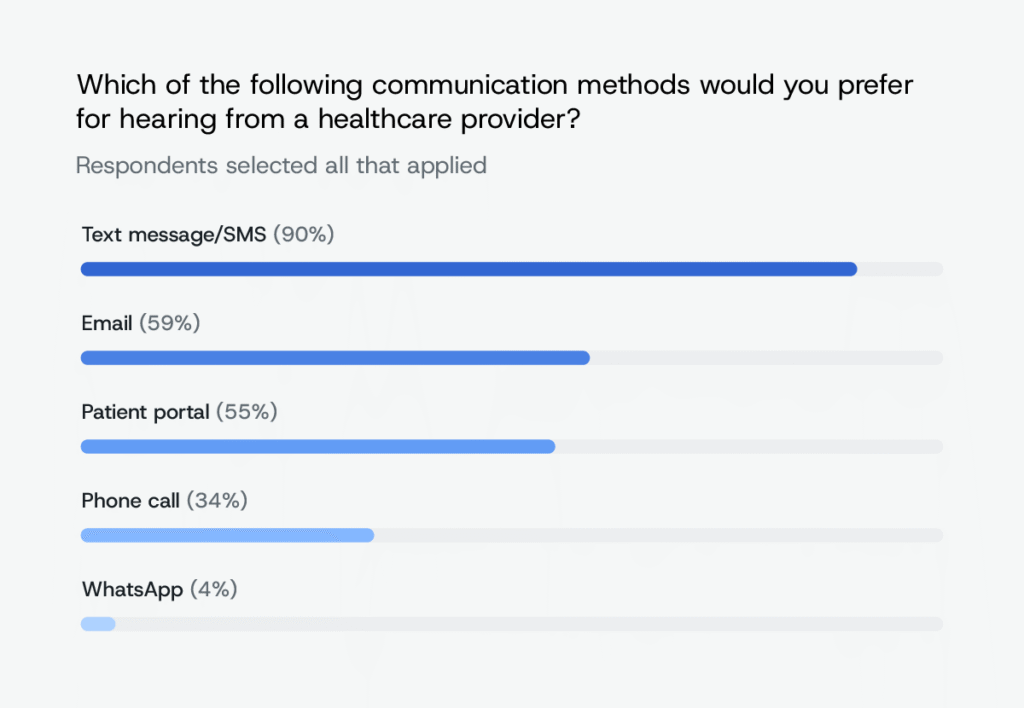
When asked which communication methods they would prefer for hearing from a healthcare provider, patients overwhelmingly chose text messaging. 90% of respondents say they prefer to receive healthcare communication by text, placing SMS well ahead of email (59%), patient portals (55%), and phone calls (34%). The results show a clear hierarchy in channel preference, with texting standing out as the most favored option for patient-provider communication in 2026.
Appointment and prescription reminders top patients’ wish lists
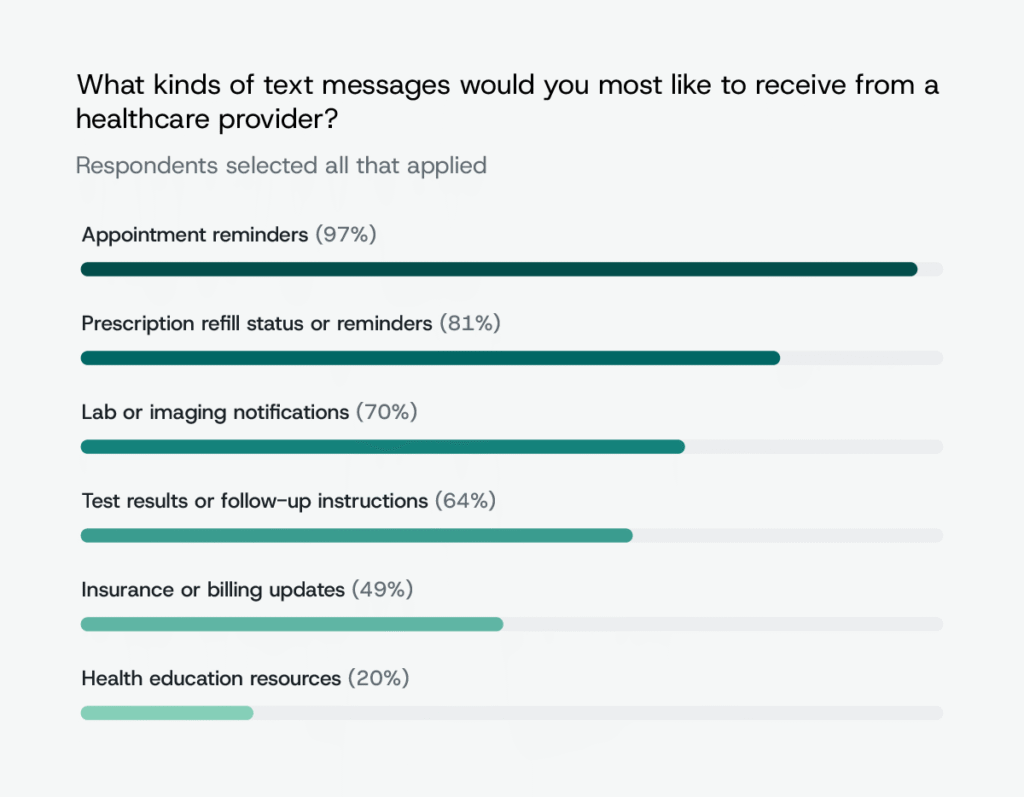
To understand what types of healthcare text messages patients actually want to receive, we asked respondents which messages they would be most likely to opt in to from providers and pharmacies. Appointment reminders clearly top the list, with 97% of patients saying they want to receive them by text, underscoring how strongly patients value messages that help keep care on track and prevent missed visits. Prescription refill updates and reminders follow closely at 81%, while 70% say they want lab or imaging notifications, pointing to particularly strong demand for SMS around time-sensitive moments when patients either need a prompt to act or are waiting for important updates.
Interest drops off when messages move away from immediate care coordination. Fewer than half of patients (49%) say they want insurance or billing updates by text, and just 20% are interested in receiving health education resources via SMS.
This preference for operational over informational messaging is reinforced when patients are asked to weigh in on importance: 88% of Americans say it is “important” or “very important” to receive appointment and prescription reminders by text from their healthcare provider or pharmacy. Gen X patients are the most likely to rate these reminders as essential (90%), and women are slightly more likely than men to consider text reminders “very important” for healthcare (42% versus 34%).
Most patients expect some personalization in healthcare texts
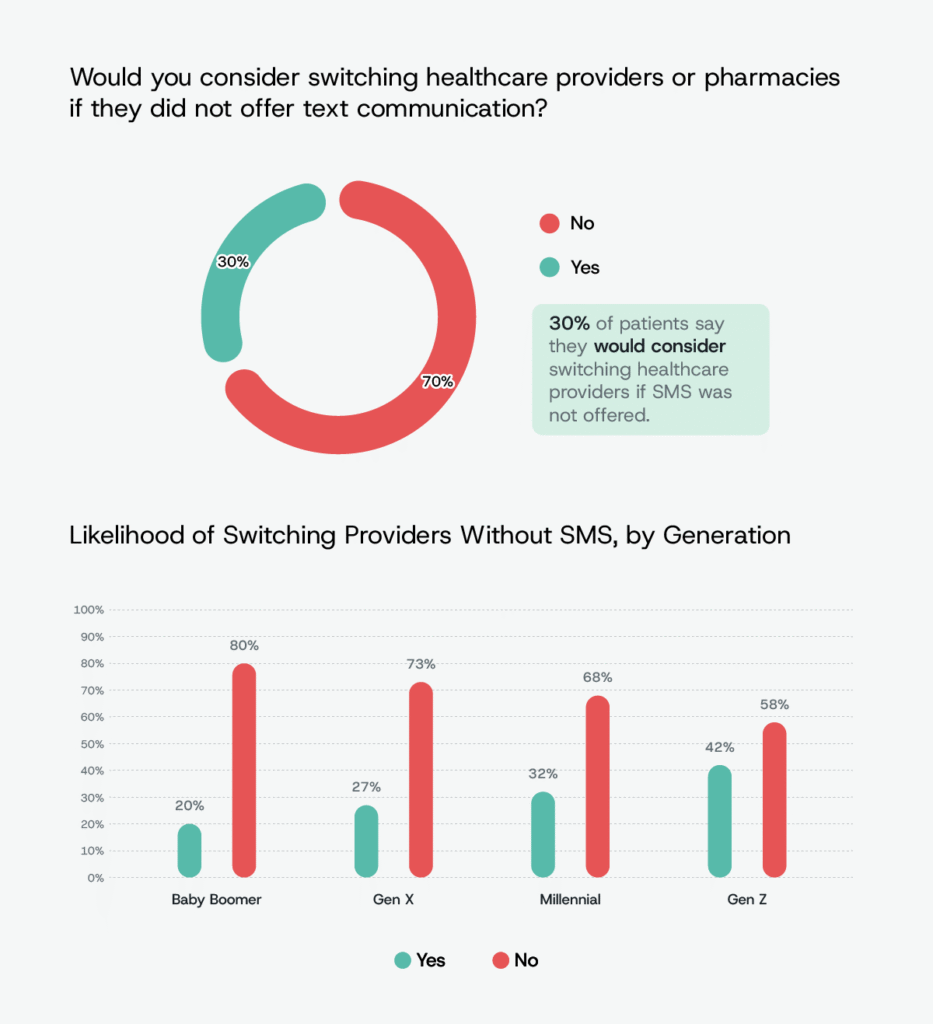
When we asked patients how the availability of text communication factors into their choice of healthcare provider, 30% of Americans said they would consider switching providers or facilities if texting were not offered. That willingness varies sharply by age. 42% of Gen Z patients say they would consider switching providers over the lack of text communication, compared with just 20% of Baby Boomers. The data suggests that Gen Z opts into healthcare texts less than other generations because they likely see the doctor less — but when they do engage with the healthcare system, they are more likely to view texting as a baseline expectation rather than a nice-to-have feature.
Expectations extend beyond whether providers offer texting to how those messages are delivered. Nearly half of Americans (48%) say healthcare text messages should be at least semi-personalized, such as including their name or specific appointment details, while only 10% say they are comfortable receiving messages with no personalization at all. Older patients appear to place even greater emphasis on this detail, with 63% of Baby Boomers expecting semi-personalized healthcare texts, compared with 45% of Gen Z patients.
Patient text messaging can reduce no-shows and boost prescription refill rates
Patient behavior is often discussed as a fixed challenge in healthcare, but our survey data suggests that communication plays a meaningful role in shaping follow-through. When we asked patients how text reminders influence their actions, the responses consistently pointed to SMS as a factor that supports scheduling, attendance, and medication adherence.
85% of Americans say they would be more likely to schedule an appointment if they received a text reminder from their healthcare provider, and 84% say they would be more likely to attend an appointment with a text reminder. The findings suggest that SMS reminders play a role at both the scheduling and follow-through stages of the care journey.
88% of patients say they would be more likely to refill a prescription if they received a text reminder, with women showing a stronger response than men (92% versus 83%). At the same time, the data highlights the consequences of missed or poorly timed communication. More than a third of Americans (34%) admit they have missed a medical appointment because they did not see or receive a reminder in time, and nearly 40% say they have missed an important healthcare message due to poor communication from a provider or facility.
Younger adults appear particularly affected, as 42% of Gen Z patients report missing appointments due to missed reminders, and more than 47% say they have missed critical healthcare messages because of communication breakdowns. Among those who missed important messages, the most common outcomes include missing or rescheduling appointments, experiencing stress or confusion, and forgetting to refill prescriptions.
Patients want two-way texting with doctors’ offices
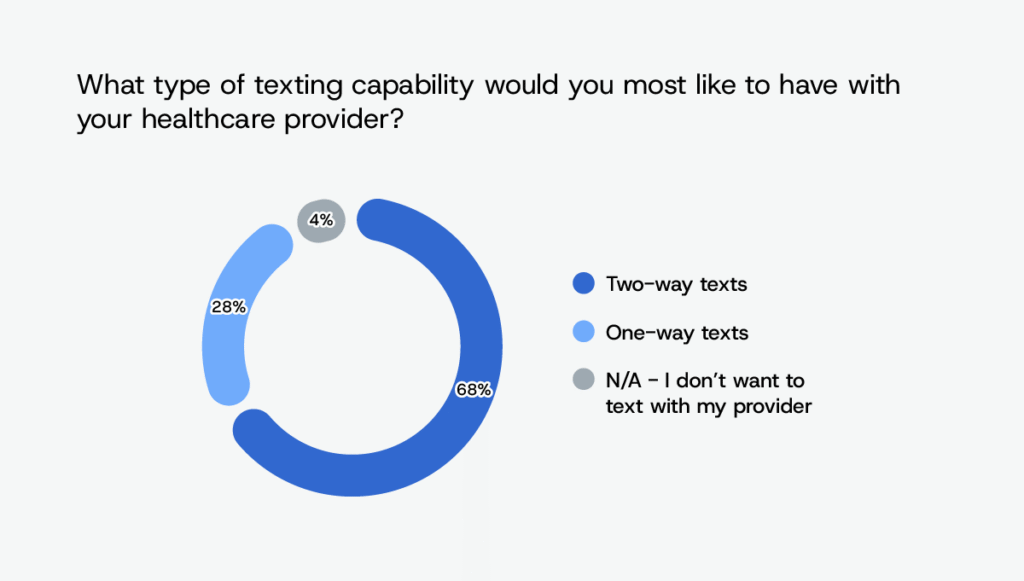
To understand whether patients see healthcare texting as a one-way notification tool or a conversational channel, we asked respondents how they would prefer to communicate with their healthcare providers. Most patients (68%) say they want two-way texting that allows them to ask simple questions or confirm or reschedule appointments, rather than receiving automated reminders they cannot respond to. Interest in two-way communication is especially strong among older adults, with 75% of Baby Boomers saying they prefer two-way texting with healthcare providers.
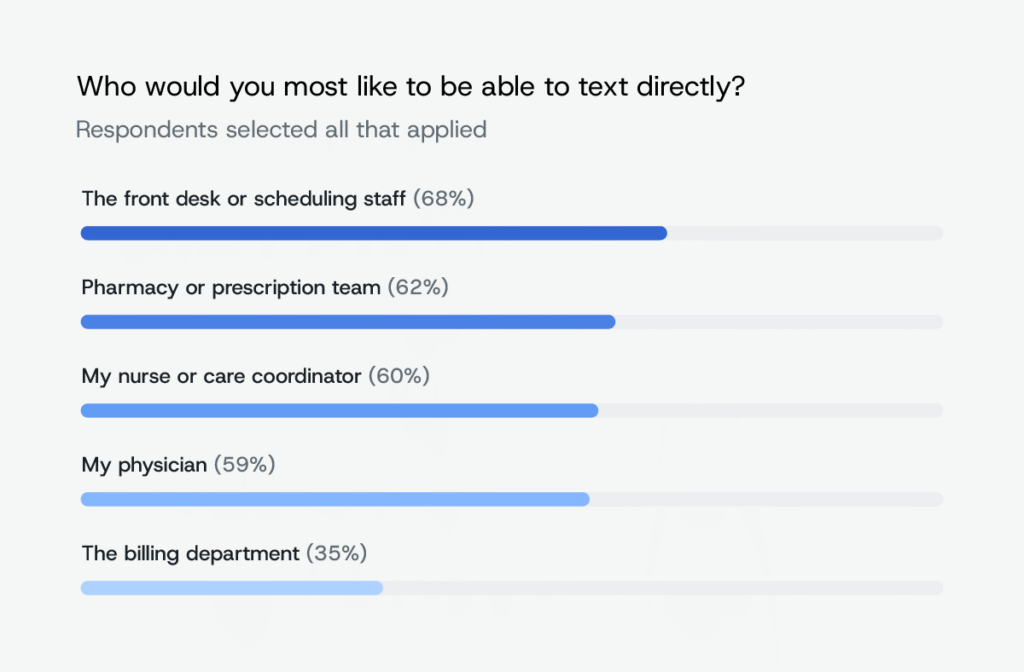
When we asked patients who they would most like to text directly within a healthcare setting, preferences clustered around roles tied to scheduling and care coordination. Front desk or scheduling staff ranked highest, with 68% of respondents saying they would want the ability to text them directly. Pharmacy or prescription teams (62%) and nurses or care coordinators (60%) followed closely. Just 35% of Americans say they would want to text directly with billing departments, suggesting that not all healthcare interactions feel equally suited for SMS.
When asked what might prevent them from opting in to healthcare texting at all, concerns about message volume top the list. 40% of patients worry they would receive too many messages or that texts would feel like spam. Still, 38% say nothing would prevent them from opting in, indicating broad openness to healthcare SMS when expectations around frequency and relevance are met. Privacy and security concerns remain a consideration for some, with 33% citing them as a potential barrier to opting in.
Automation with empathy: when patients want a real person
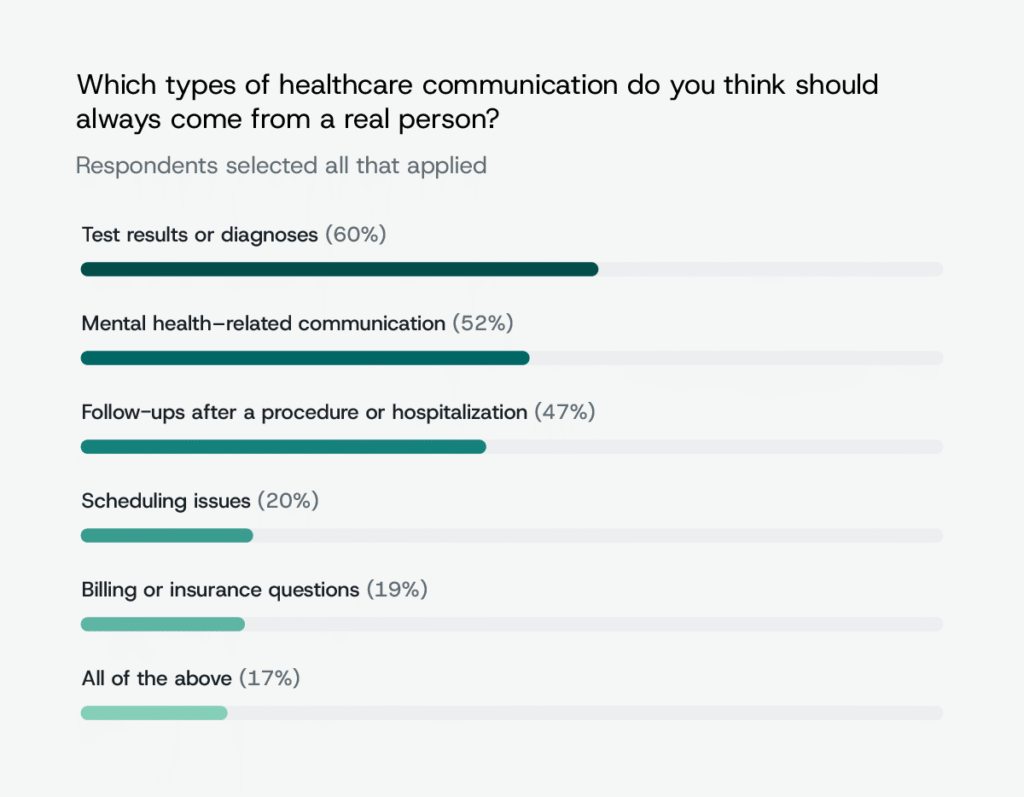
To better understand where automation fits in healthcare communication — and where it does not — we asked patients which types of messages they believe should always come from a real person. Sensitive healthcare topics clearly stand apart. 60% of respondents say test results or diagnoses should always be delivered by a human, while 52% feel the same about mental health discussions and 47% about follow-ups after medical procedures or hospitalizations.
At the same time, concerns about trust and security do not appear to be a major barrier to healthcare texting overall. Nearly 80% of Americans say they are either “confident” or “very confident” that healthcare providers can protect their personal information when communicating over text. Confidence levels vary slightly by generation, with Gen Z patients reporting the highest levels of trust and Millennials expressing the least.
Patients want speed and convenience, but not at the expense of a human
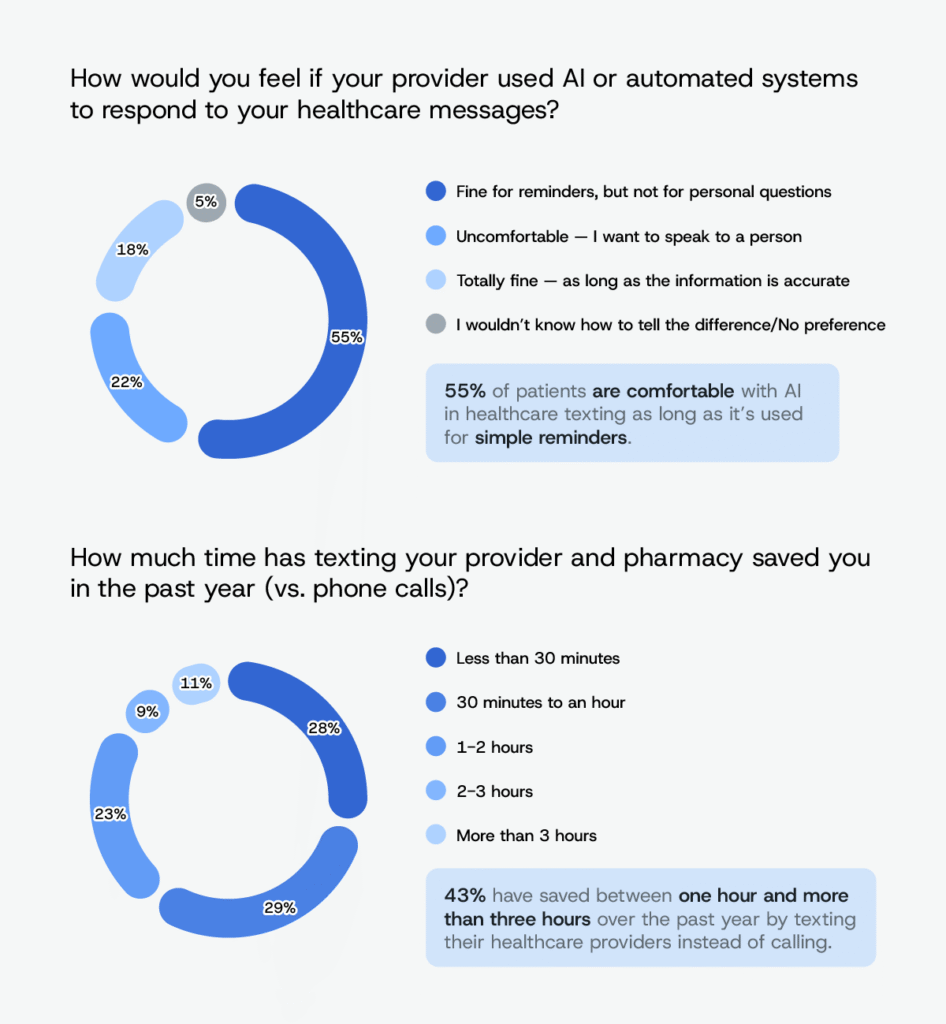
There is no question that AI is becoming increasingly integrated into the healthcare system, and healthcare communication is no exception. When we asked patients how they feel about AI or automated systems responding to healthcare messages, most (55%) say they are comfortable with automation when it is used for simple reminders or routine updates, but that comfort drops off for personal or sensitive conversations. At the same time, 22% say they are uncomfortable with AI chatbots for patient text messaging and want to communicate with a real person, while 18% say they are fully comfortable with automation as long as the information provided is accurate.
Despite these boundaries, patients clearly associate text-based communication with efficiency: 43% say they saved between one hour and more than three hours over the past year by texting their healthcare providers instead of calling, and 78% expect a same-day response when they reach out. The findings suggest that while patients value speed and convenience, they still expect human involvement when communication requires judgment, context, or empathy.
Better patient communication starts with meeting expectations
If there’s one clear takeaway from this research, it’s that patient communication has become inseparable from the healthcare experience itself. Text messaging now sits at the center of how patients expect to schedule care, receive reminders, and stay connected to providers, while preferences for two-way communication, personalization, and timely responses reflect rising expectations across every stage of the care journey.
At the same time, the data shows that progress does not mean replacing people with technology. Patients welcome automation when it simplifies routine interactions, but they continue to expect empathy, judgment, and human involvement when conversations become personal or sensitive. The healthcare organizations that succeed in 2026 will be the ones that balance speed and convenience with trust, clarity, and responsiveness.
Sinch Engage conducted this research to better understand how secure, scalable messaging can support stronger patient-provider communication without sacrificing experience or privacy. Learn how healthcare organizations are using secure text messaging for healthcare to improve engagement, reduce no-shows, and meet evolving patient expectations.
Methodology
Ahead of 2026, Sinch Engage surveyed 1,000 patients across the U.S. between December 4 and 7, 2025. Respondents ranged in age from 18 to 78 and represented a broad mix of demographics and geographic regions nationwide.
The survey examined patient preferences and behaviors related to healthcare communication, including:
- Texting habits
- Appointment and prescription reminders
- Two-way messaging
- Privacy concerns
- Attitudes toward automation and AI in healthcare messaging
Results are based on self-reported responses and analyzed in aggregate to identify overall trends in patient communication.
Fair Use
You are welcome to use, reference, and share non-commercial excerpts of this study with proper attribution. If you cite or cover our findings, please link back to this page so readers can view the full methodology, charts, and context.
